#symptoms of neurological diseases in dogs
Explore tagged Tumblr posts
Link
This is an article about neurological diseases in dogs
#pet_care #petlovers #pet #pets
0 notes
Text
Recognizing Early Signs of Canine Distemper in Dogs
Canine Distemper is a serious and often fatal disease that affects dogs worldwide. Caused by the Canine Distemper Virus (CDV), this highly contagious disease can spread rapidly among unvaccinated dogs, leading to severe health complications. Recognizing the early signs of Canine Distemper Disease is crucial for ensuring prompt veterinary care and improving the chances of recovery.

What is Canine Distemper?
Canine Distemper is a viral disease that affects a dog’s respiratory, gastrointestinal, and nervous systems. The virus is primarily spread through airborne exposure (e.g., sneezing or coughing) and direct contact with infected animals or contaminated objects. Puppies and unvaccinated dogs are especially vulnerable to the disease.
Early Signs of Canine Distemper
Early detection of Canine Distemper can make a significant difference in the outcome for your dog. Here are some of the initial signs to watch for:
Fever: One of the first signs of Canine Distemper is a sudden onset of fever. This initial fever may be mild and go unnoticed, but it can return with greater intensity. Monitoring your dog’s temperature regularly can help detect this early sign.
Eye Discharge: Clear or watery discharge from the eyes is another common early symptom. This discharge can quickly become thick, yellow, and crusty as the disease progresses. Your dog’s eyes may also appear red and swollen.
Nasal Discharge: Similar to the eye discharge, dogs with Canine Distemper may develop a runny nose. This nasal discharge may start as clear but can become thick and pus-like, indicating an infection.
Coughing and Sneezing: The Canine Distemper Virus often affects the respiratory system, leading to coughing, sneezing, and difficulty breathing. These symptoms can be mistaken for kennel cough or other respiratory infections, so it’s important to seek veterinary advice if they persist.
Lethargy: Dogs in the early stages of Canine Distemper often exhibit signs of lethargy and depression. If your dog seems unusually tired, uninterested in activities, or is sleeping more than usual, it could be an early indication of the disease.
Loss of Appetite: A decrease in appetite or refusal to eat is a common early symptom. Dogs with Canine Distemper may also experience weight loss due to their reduced food intake.
Vomiting and Diarrhea: Gastrointestinal symptoms such as vomiting and diarrhea can occur in the early stages. These symptoms can lead to dehydration, so it’s important to ensure your dog stays hydrated and seek veterinary care promptly.
Hardening of Paw Pads and Nose: In some cases, dogs with Canine Distemper develop a condition known as hyperkeratosis, which causes the paw pads and nose to harden and thicken. This is a more advanced sign but can occur early in the disease’s progression.
What to Do if You Suspect Canine Distemper
If you notice any of these early signs of Canine Distemper in your dog, it is crucial to seek veterinary care immediately. Early intervention can make a significant difference in the prognosis and treatment outcomes. Tri-County Animal Hospital offers comprehensive diagnostic and treatment services to manage Canine Distemper Disease effectively.
Diagnosing Canine Distemper
Veterinarians diagnose Canine Distemper through a combination of clinical signs, medical history, and laboratory tests. Blood tests, polymerase chain reaction (PCR) tests, and antibody tests are commonly used to confirm the presence of the Canine Distemper Virus. Prompt and accurate diagnosis is essential for initiating appropriate treatment and care.
Preventing Canine Distemper
The best way to protect your dog from Canine Distemper is through vaccination. Puppies should receive their first distemper vaccine at six to eight weeks of age, followed by booster shots every three to four weeks until they are 16 weeks old. Adult dogs should receive regular booster shots as recommended by their veterinarian. Tri-County Animal Hospital can provide guidance on an appropriate vaccination schedule for your dog.
Conclusion
Recognizing the early signs of Canine Distemper in dogs is vital for ensuring timely and effective treatment. If you notice any symptoms such as fever, eye or nasal discharge, coughing, lethargy, loss of appetite, vomiting, diarrhea, or hardening of the paw pads and nose, seek veterinary care immediately. Early diagnosis and intervention, along with preventive measures like vaccination, are key to protecting your dog from this serious disease. For expert care and advice on Canine Distemper, contact Tri-County Animal Hospital today to schedule an appointment.
#Canine Distemper#Canine Distemper Virus#Canine Distemper Disease#Early Signs of Canine Distemper#Symptoms of Canine Distemper#Dog Health#Pet Health#Tri-County Animal Hospital#Dog Fever#Dog Respiratory Symptoms#Dog Gastrointestinal Issues#Dog Eye Discharge#Dog Lethargy#Dog Neurological Symptoms#Canine Distemper Prevention#Canine Distemper Treatment#Dog Vaccination#Veterinary Care#Pet Care#Canine Distemper Diagnosis
0 notes
Text
COVID-19's long-term effects on the body: an incomplete list
COVID’s effect on the immune system, specifically on lymphocytes:
NYT article from 2020 (Studies cited: https://www.biorxiv.org/content/10.1101/2020.05.18.101717v1, https://www.biorxiv.org/content/10.1101/2020.05.20.106401v1, https://www.unboundmedicine.com/medline/citation/32405080/Decreased_T_cell_populations_contribute_to_the_increased_severity_of_COVID_19_, https://www.medrxiv.org/content/10.1101/2020.06.08.20125112v1)
https://www.biorxiv.org/content/10.1101/2022.01.10.475725v1
https://www.science.org/doi/10.1126/science.abc8511 (Published in Science)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9057012/
https://www.forbes.com/sites/williamhaseltine/2022/04/14/sars-cov-2-actively-infects-and-kills-lymphoid-cells/
https://www.cleveland.com/news/2022/10/in-cleveland-and-beyond-researchers-begin-to-unravel-the-mystery-of-long-covid-19.html
SARS-CoV-2 infection weakens immune-cell response to vaccination: NIH-funded study suggests need to boost CD8+ T cell response after infection
https://www.merckmanuals.com/professional/hematology-and-oncology/leukopenias/lymphocytopenia
https://thetyee.ca/Analysis/2022/11/07/COVID-Reinfections-And-Immunity/
Dendritic cell deficiencies persist seven months after SARS-CoV-2 infection
https://www.frontiersin.org/articles/10.3389/fimmu.2022.1034159/full
https://www.n-tv.de/politik/Lauterbach-warnt-vor-unheilbarer-Immunschwaeche-durch-Corona-article23860527.html (German Minister of Health)
Anecdotal evidence of COVID’s effects on white blood cells:
https://twitter.com/DrJohnHhess/status/1661837956875956224
https://x.com/TristanVeness/status/1661565201345564673
https://twitter.com/TristanVeness/status/1689996298408312832
Much more if you speak to Long Covid patients directly!
Related information of interest:
China approves Genuine Biotech's HIV drug for COVID patients
COVID as a “mass disabling event” and impact on the economy:
https://www.ctvnews.ca/health/report-says-long-covid-could-impact-economy-and-be-mass-disabling-event-in-canada-1.6306608
https://x.com/inkblue01/status/1742183209809453456?s=20
COVID’s impact on the heart:
https://www.dailystar.co.uk/news/world-news/deadly-virus-could-lead-heart-31751263 (Research from: Japan's Riken research institute)
https://www.brisbanetimes.com.au/national/queensland/unlike-flu-covid-19-attacks-dna-in-the-heart-new-research-20220929-p5bm10.html
https://www.mdpi.com/2077-0383/12/1/186
https://medicalxpress.com/news/2023-04-mild-covid-effects-cardiovascular-health.html
https://publichealth.jhu.edu/2022/covid-and-the-heart-it-spares-no-one
https://www.bhf.org.uk/informationsupport/heart-matters-magazine/news/coronavirus-and-your-health/is-coronavirus-a-disease-of-the-blood-vessels (British Heart Foundation)
COVID’s effect on the brain and cognitive function:
https://www.openaccessgovernment.org/article/brain-infection-by-sars-cov-2-lifelong-consequences/171391/
https://www.cidrap.umn.edu/covid-19/study-shows-covid-leaves-brain-injury-markers-blood
https://www.theguardian.com/world/2020/jul/08/warning-of-serious-brain-disorders-in-people-with-mild-covid-symptoms
Cognitive post-acute sequelae of SARS-CoV-2 (PASC) can occur after mild COVID-19
Neurologic Effects of SARS-CoV-2 Transmitted among Dogs
https://journals.lww.com/nsan/fulltext/2022/39030/neurological_manifestations_and_mortality_in.4.aspx
https://www.salon.com/2023/06/17/new-evidence-suggests-alters-the-brain--but-the-extent-of-changes-is-unclear/
https://www.scientificamerican.com/article/covid-virus-may-tunnel-through-nanotubes-from-nose-to-brain/
https://neurosciencenews.com/post-covid-brain-21904/
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(22)00260-7/fulltext
https://medicalxpress.com/news/2022-08-covid-infection-crucial-brain-regions.html
https://news.ecu.edu/2022/08/04/covid-parkinsons-link/
Covid as a vascular/blood vessel disease:
https://www.salon.com/2020/06/01/coronavirus-is-a-blood-vessel-disease-study-says-and-its-mysteries-finally-make-sense/
https://www.salon.com/2023/12/27/brain-damage-caused-by-19-may-not-show-up-on-routine-tests-study-finds/
https://www.nih.gov/news-events/news-releases/sars-cov-2-infects-coronary-arteries-increases-plaque-inflammation
https://www.mdpi.com/2077-0383/12/6/2123
https://www.sciencedaily.com/releases/2021/10/211004104134.htm (microclots)
Long Covid:
Post-COVID-19 Condition in Canada: What we know, what we don’t know, and a framework for action
https://www.ctvnews.ca/health/coronavirus/more-than-two-years-of-long-covid-research-hasn-t-yielded-many-answers-scientific-review-1.6235227
https://www.cbc.ca/news/canada/london/cause-of-long-covid-symptoms-revealed-by-lung-imaging-research-at-western-university-1.6504318
https://www.cbc.ca/news/canada/montreal/long-covid-study-montreal-1.6521131
https://news.yale.edu/2023/12/19/study-helps-explain-post-covid-exercise-intolerance
Other:
- Viruses and mutation: https://typingmonkeys.substack.com/p/monkeys-on-typewriters
Measures taken by the rich and world leaders
Heightened risk of diabetes
https://jamanetwork.com/journals/jama/fullarticle/2805461
https://www.nature.com/articles/d41586-022-00912-y
Liver damage:
https://timesofindia.indiatimes.com/city/mumbai/46-of-covid-patients-have-liver-damage-study/articleshow/97809200.cms?from=mdr
tl;dr: covid is a vascular disease, not a respiratory illness. it can affect your blood and every organ in your body. every time you're reinfected, your chances of getting long covid increase.
avoid being infected. reduce the amount of viral load you're exposed to.
the gap between what the scientific community knows and ordinary people know is massive. collective action is needed.
#putting this somewhere at least as reference for... somebody hopefully#covid#disability#y'all. it is bleak out there but some very good people are doing their best to help#we need as many people aware and helping as possible
464 notes
·
View notes
Text
I saw some mentions of rabies going around again and have no clue what's set it off this time, but given recent scientific developments I want to revisit the idea of curing symptomatic rabies.
First things first: there is still no practical way to do this. The famous Milwaukee Protocol fails far more frequently than it succeeds, and even the successes are not making it out in anything like a normal state. It's been argued that it should no longer be considered a valid treatment [1] due to these issues; any continued use is because there's literally nothing else on the table.
However. There are now two separate studies showing it's possible to cure rabies in mice after the onset of symptoms. The lengths you have to go to in order to pull this off are drastic, to put it mildly, and couldn't really be adapted to humans even if you wanted to. But proof of concept is now on the board.
long post under the cut, warnings for animal experimentation and animal death. full bibliography at the end and first mention of each source links to paper.
Quick recap - rabies is a viral disease of mammals usually transmitted through the saliva of an infected animal. From a contaminated bite wound, it propagates slowly for anywhere from days to months until it reaches the central nervous system (CNS). Post-exposure vaccination can head it off during this phase, but once it reaches the CNS and neurological symptoms appear it's game over. There will typically be a prodromal phase where the animal doesn't act right - out at the wrong time of day, disoriented, abnormally friendly, etc. This will then progress to the furious (stereotypical "mad dog" disease) and/or paralytic phases, with death eventually caused by either seizures or paralysis of the muscles needed for breathing.
That's the course we're familiar with in larger animals. Mice, though, are fragile little creatures with fast metabolisms.
In the first study's rabies infection model, lab mice show rabies virus in the spinal cord by day 4 after infection and in the brain by day 5. Weight loss and slower movement start by day 7, paralysis starting from the hind limbs from day 8 on, and if not euthanized first they're dead by day 10-13. [2]
This study (fittingly conducted at the Institut Pasteur) had two human monoclonal antibodies, and wanted to see if there was any possibility they could be used to cure rabies after what we think of as the point of no return.
Injecting the antibodies into muscle saved some mice if done at days 2 or 4, and none if done later, even at high doses of 20 milligrams per kilogram of body weight of each. Conclusion: targeting the virus out in the rest of the body is no use if it's already replicating in the CNS.
Getting a drug past the blood-brain barrier is, to use a highly technical term, really fucking hard. It's the sort of problem that even the best-funded labs and biggest companies in the world routinely fail at. And that's for small molecule drugs, which are puny compared to antibodies.
But this isn't drug development for a clinical trial. This is a very, very early proof-of-concept attempt, which means you're willing to ignore practicality to see if this idea is even remotely workable. So you can do things like brute force the issue by cutting through the skull to implant a microinfusion pump, which lets you deliver the antibodies directly into the normally-protected space around the brain. Combine this with the normal injections, and you can treat both the CNS and the rest of the body at the same time. Here's a survival graph of treated mice. X axis is days, Y axis is percentage of mice in that group still alive.
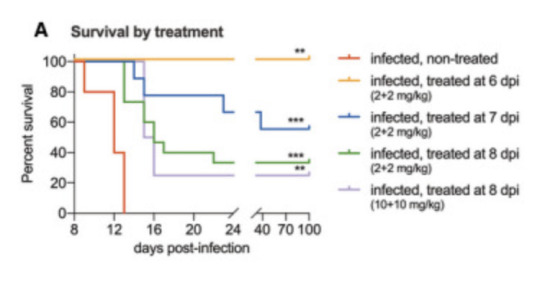
Figure 2A from reference 2, accessed February 2024
The fact that the blue, green, and purple lines did anything other than sink horribly to zero is unheard of. When the combination treatment was started at day 6, 100% of the mice survived. Started at day 7 (prodromal phase), 5 out of 9 mice recovered and survived. Started at day 8 (solidly symptomatic, paralysis already starting to set in), 5 of 15 mice recovered and survived. And when they say "survived", they kept these mice all the way to day 100 to make sure. Some of them had permanent minor paralysis but largely they were back to being normal mice doing normal mouse things. So, success, but by pretty extreme means.
Enter the second paper [3]. This was a different approach using a single human monoclonal antibody against Australian bat lyssavirus (ABLV - closely related to rabies, similar symptoms in humans) to try for a cure without needing to deliver treatments directly into the CNS. They also made a luminescent version of ABLV that let them directly image viral activity, so they could see both where the virus was replicating and how much there was in a live mouse.

Figure 1 from reference 3, accessed February 2024
Mice infected with ABLV start showing symptoms around day 8. You can see in the figure that at day 3 there's viral replication in the foot at the site of infection, which has shifted into the spine and brain by day 10. So what happens if you give one of these doomed mice one single injection of the antibody into the body?
Done at day 3, the virus doesn't make it to the brain until day 14, and while disease does set in after that around 30% of the mice survive. Days 5 and 7 are much more interesting. Those mice still develop symptoms at day 8, but the imaging shows the amount of virus in their spines and brains never gets anywhere near the levels seen in untreated controls, and within days it starts to decrease. Around 80% of day 5 and 100% of day 7 mice survive.
Okay, sure, you can stop another lyssavirus, but technically you did start treatment before symptoms appeared. What about symptomatic rabies?
The rodent-adapted rabies strain CVS-11 starts causing symptoms as early as day 3 after infection, and untreated mice die between days 8 and 11. The same single dose of antibody saved 67% of mice treated on day 5 and 50% of mice treated on day 7. Without making the luminescent version of the virus there's no real-time imaging of the infection, but you can still track symptoms.
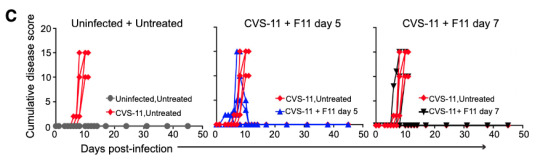
Figure 2 from reference 3, accessed February 2024. CVS-11 is the name of the rodent rabies strain and F11 is the name of the antibody.
Disease score is a combination of several metrics including things like whether the mice are behaving normally and whether they show signs of paralysis. In untreated mice it goes up and up, and then they die. If one of those lines starts coming back down and continues past day 10 or so, that's a mouse that recovered. The success rate isn't as good as against ABLV, but again, this is a rabies strain specifically adapted to rodents and treatment wasn't started until it was well-established in the CNS.
So how on earth is this happening? The antibody neutralizes both ABLV and rabies really well in a test tube, but we've already established that there's no way a huge lumbering antibody is making it past the blood-brain barrier without serious help. Something about the immune response is clearly making it in there though. And it turns out that if you start trying this cure in mice missing various parts of their immune systems, mice without CD4+ T cells don't survive even with the treatment. By contrast mice without CD8+ T cells take longer to work through the infection, but they eventually manage it and are immune to reinfection afterwards.
To grossly oversimplify the immune system here, CD4+ are mature helper T cells, which work mostly by activating other immune cells like macrophages (white blood cells) and CD8+ T cells (killer T cells) against a threat.
Normally, T cells are also kept out by the blood-brain barrier, but we know that in certain specific cases including viral infection they can pass it to migrate into the brain. In the brains of the infected mice for which antibody treatment either wasn't given or didn't work, you can find a roughly even mix of CD8+ and CD4+ T cells along with a whole lot of viral RNA. But in the brains of those successfully fighting off the infection, there's less viral RNA and the cells are almost exclusively CD4+. So the antibody doesn't work by neutralizing the virus directly - something about it is activating the animal's own immune system in a way that gives it a fighting chance.
Again, neither of these proof of concept treatments is really workable yet as a real world cure. The first one is almost hilariously overkill and still has a pretty good chance of failure. The second is less invasive but careful sequencing still shows both low-level viral replication and signs of immune response in the brains of the survivors even at day 139, so it may not be truly clearing the virus so much as trading a death sentence for life with a low-level chronic infection. But now we know that 1. curing rabies after symptoms begin is at least theoretically possible, and 2. we have some clues as to mechanisms to investigate further.
Not today. Not tomorrow. But maybe not never, either.
References:
Zeiler, F. A., & Jackson, A. C. (2016). Critical appraisal of the Milwaukee protocol for rabies: this failed approach should be abandoned. Canadian Journal of Neurological Sciences, 43(1), 44-51.
de Melo, G. D., Sonthonnax, F., Lepousez, G., Jouvion, G., Minola, A., Zatta, F., ... & Bourhy, H. (2020). A combination of two human monoclonal antibodies cures symptomatic rabies. EMBO molecular medicine, 12(11), e12628.
Mastraccio, K. E., Huaman, C., Coggins, S. A. A., Clouse, C., Rader, M., Yan, L., ... & Schaefer, B. C. (2023). mAb therapy controls CNS‐resident lyssavirus infection via a CD4 T cell‐dependent mechanism. EMBO Molecular Medicine, 15(10), e16394.
319 notes
·
View notes
Text
A story about a prion disease apocalypse could be so fucked up fun.
Perhaps the disease has been spreading for a while, but appeared to not harm humans like CWD, or it's an entirely new one that a cow just developed one day. It can spread through their waste, their spit, their blood. Quite a few animals have already been infected by the time the first few enter the human food chain.
It's another while before the new prion disease is noticed; people aren't getting sick, and it takes a while before infected animals show symptoms. Eventually the weird symptoms are noticed, and the new disease is found, but it's already too late. It's spread so far that it proves very difficult to stamp out no matter how many infected animals get destroyed, and every day it isn't wiped out means more humans coming into contact with the prions. Although right now, no-one knows for sure if it can even jump the species barrier.
A few years later, it starts. A few people with mysterious and deadly neurological issues here and there, who's autospies reveal their brains have been turned to sponge. The numbers slowly climb upwards with each year. It's still spreading in farm animals.
Efforts to resist the disease increase; there isn't any treatment, but there are better tests. Through these it's discovered that not only are carrier animals that can spread the disease everywhere, but an eyewatering percentage of the population harbour the abnormal prions too- spreading not just through tainted food at this point, but also blood transfusions and surgical instruments. Even the water in the worst affected places isn't safe any more. Reassurances that not everyone will develop the prion disease are no comfort for many.
Every year the numbers climb. It goes from a very rare illness, to an unusual one, to one that's so common that you probably know someone who got killed by it. Attempts at a cure all fail, no matter how promising they seem. A suffocating cloak of dread falls over the world, even as many people try to ignore it and go about their daily lives. It isn't uncommon now to see someone with obvious symptoms who is in denial. Not that confronting their death head on would help; healthcare is underfunded and overwhelmed, they would be waiting months for anything that might alleviate their suffering.
The collapse begins a decade into the pandemic. People are dying left, right and centre, even children who weren't born when it first began to spread; it might have spread to them in the womb, but there are so few scientists left and they're so focused on finding a cure that not much research is done. Take a walk in a city and you'll see dozens of empty buildings and massive queues by the hospitals. Walk in the countryside and you'll probably see a half dead animal wracked with spasms. Mammals have become rarer; even dogs and cats are a bit unusual to see. Anything that hasn't reduced in numbers is studied intently to discover its secrets, all to no avail.
Infrastructure begins break down; there aren't many people left to maintain it, and a lot of them aren't well. Medical care is borderline impossible to get because there's so many people and so few living doctors and nurses; more and more people are dying of curable afflictions without ever being seen. Food is scarce because animal products are off the menu and it's nigh impossible to transport and grow food when so many people have died. Costs shoot up, and people protest because no-one can afford the prices- especially when not that many people work any more, being too ill to work or having to care for their ill loved ones. The only thing that gets cheaper is housing.
Protesting does help, and resources are more evenly distributed in the last few years. But there's still nothing that can be done for the illness, and the sick are actually dying faster because some places now have no medical staff. Medicines get scarce as manufacturing plants shut down for want of staff. Whole regions lose their electricity as the final workers are forced to turn off the grid lest the power plant cause a disaster once the prion disease has killed them. Governments can't fill the empty seats in their parliaments, and high voter turnout amounts to thousands of people casting their ballots. Quite a few governments just throw in the towel at that point. In places with newspapers, it isn't uncommon for them to run emotional stories about people from areas so badly hit that they thought they could be the last living people.
Eventually things begin to level out. A couple of people were lucky enough to never be exposed, or to have some resistance. It's the same for other mammals, although they're scarce and many are extinct. Most areas are forced into subsistence farming on poisoned land, without the help of domesticated animals. Most strive to rebuild, but to some it seems like the final, tortured days before the end.
27 notes
·
View notes
Text
Foreman brings House a case.
This alone is enough to catch House's (begrudging) attention, since usually it's Cameron coming to him with sob stories and puppy-dog eyes. Not that Foreman bothers with either.
The case was brought to him by a colleague he knows through various neurology conferences over the years. Her patient is late twenties, male, lives an unremarkable life as a computer tech. Symptoms: debilitating migraines, audio-visual hallucinations, short-term memory loss, and what seem to be intense night terrors. All of which the patient denies or insists aren't cause for concern.
"TBI or neurodegenerative disease. Boring."
"That's what I thought too," Foreman says, "until I saw these."
fMRIs. EEGs. There's a handful of them, and they're like nothing House has ever seen before. Brain activity in places that brains aren't usually active. House cracks a joke about mutants and Professor X, but Foreman can tell: he's got him. He's interested now. He wants to see the patient, run some scans of his own.
"That's the thing. He's not here, he's in California."
"Well, Cuddy vetoed my request to purchase Cerebro for the department, so..."
"He insists there's nothing wrong with him. We wouldn't even have these scans if his sister hadn't guilted him into letting her get some imaging."
"Hallucinations, memory loss, night terrors, and he's not worried at all. Sounds like a liar. My favourite." House squints at the patient info attached to the scans. "Fine. Tell Cuddy we're taking a field trip to see one Charles Bartowski."
#fudging the timeline a bit here but the idea wouldn't leave me alone#to be clear: this is when the intersect is fucking with chuck's head but before ellie knows what's going on#i can only imagine the changes wrought by the intersect could look something wild on imaging#but also I know bugger all about medicine so take everything I say with a grain of salt#house md#chuck tv#chuck bartowski#nbc chuck
45 notes
·
View notes
Note
What other diseases can you smell? Does schizophrenia have a smell?
Not as far as I've identified yet. I haven't spent a lot of time around (known) schizophrenic folks in person, so I won't rule it out completely as a possibility, but the common thread in what I can smell seems to be damage to the nervous system. My understanding of schizophrenia is that it's more of a neurotype issue than a damage one? Also I can't smell old neurologic damage that left permanent issues behind, only currently-occurring, so even if it were a damage-related disorder it would only possibly work if that damage were continuing to happen or had very recently happened.
I can smell seizure disorders, but only shortly before and after an actual seizure occurs (and I can't tell the difference between impending and past, unless I have information about when the last time that person had a seizure was to know if it was within the lingering-smell window). Someone with a well-controlled seizure disorder does not have a distinct smell to me the vast majority of the time. Most consistently I can smell chronic neuro-degenerative diseases (alzheimer's, parkinsons), occasionally particularly severe migraines, and sometimes also diabetic neuropathy when it's particularly bad.
And as mentioned in the tags on that post, covid definitely has a distinctive smell as well. Not the virus itself, but, the smell that comes off of a person with an active infection that's attacking their nervous system -- the person I found this out due to was experiencing atypical symptoms, with intense bouts of vertigo as the primary issue rather than respiratory symptoms, and hadn't identified the illness as covid yet. Unfortunately I also caught covid pretty soon after that, whooops but now I know to actually GTFO anytime I catch THAT smell on someone in the future!
I consider this my second-most-useless superpower because usually by the time I can smell it without getting closer than is generally socially acceptable whoever's got the issue already knows about it, and even if I do manage to sniff an impending seizure or early-stage something or other and warn the person, what cause do they have to believe me? I mean everyone knows that seizure-alert dogs are a thing but generally humans are assumed to not have sensitive enough noses for that.
7 notes
·
View notes
Text
The Impact of Rabies on the Endocannabinoid System: Unraveling the Connection
World Rabies Day 28th September
Introduction
Rabies, a deadly viral disease that affects the nervous system, has long been a cause for concern worldwide. While its effects on the central nervous system are well-documented, recent research has shed light on the impact of rabies on the endocannabinoid system. This article aims to explore this intriguing connection and understand how rabies affects the delicate balance of the endocannabinoid system.
Understanding Rabies
Rabies is primarily transmitted through the bite or scratch of an infected animal, typically dogs, bats, or other wildlife. Once the virus enters the body, it travels to the brain, causing inflammation and neurological symptoms. Rabies can be classified into two forms: furious rabies, characterized by aggressive behaviour, and paralytic rabies, which leads to muscle weakness and paralysis.
The Endocannabinoid System
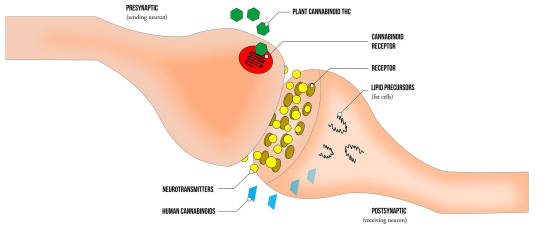
The endocannabinoid system (ECS) is a complex network of receptors, endocannabinoids, and enzymes that play a crucial role in maintaining homeostasis within the body. It regulates various physiological processes such as pain sensation, mood, appetite, and immune response. The ECS consists of two main receptors, CB1 and CB2, which are found throughout the body, including the brain.
Impact of Rabies on the Endocannabinoid System
Recent studies have indicated that rabies infection can disrupt the functioning of the endocannabinoid system. The virus affects the CB1 receptors in the brain, leading to altered neurotransmission and impaired signalling. This disruption may contribute to the behavioural changes observed in individuals infected with rabies, such as aggression and hyperactivity.
Inflammation and Immune Response

Rabies infection triggers a robust inflammatory response in the brain, leading to encephalitis. This inflammation can further impact the endocannabinoid system, as inflammatory mediators can interfere with the normal functioning of CB1 receptors. The dysregulation of the ECS due to inflammation may contribute to the neurological symptoms associated with rabies.
Conclusion
The connection between rabies and the endocannabinoid system highlights the intricate relationship between viral infections and the body's regulatory systems. While much remains to be discovered, studying the impact of rabies on the ECS may provide valuable insights into the development of novel treatment strategies. By unravelling this complex interplay, researchers can pave the way for improved outcomes for individuals affected by this devastating disease.
#rabies#rabies awareness#endocannabinoidsystem#endocannabinoids#cannabis#cbd#health#feelgreatagain#budandtender
2 notes
·
View notes
Text
São Paulo Registers First Case of Canine Rabies in 40 Years
Infection was confirmed by the Pasteur Institute in an animal rescued in the city

The city of São Paulo confirmed on Friday (1st) the first case of canine rabies since 1983.
The dog infected by the disease had been rescued a few days before in the Butantã neighborhood, showing neurological symptoms. The animal died a day after receiving veterinary care.
Continue reading.
3 notes
·
View notes
Text


sorry this is just me rambling about veterinary stuff & i don't remember how to do a read more or if tumblr even has that function. it's nothing major or terrible
so bubo's got a lot going on right now. he spent a couple nights in the hospital last month with bronchitis/asthma (main symptom was abdominal breathing; cats should not be breathing so hard that they have to use their abs to move air in & out of their lungs). while he was there they also diagnosed him with hyperthyroidism & lymphocytosis based on blood work. this is on top of his prior history of head trauma, neurological damage, feline viral rhinotracheitis, eosinophilic granuloma complex, food allergies that cause his skin to get red & angry & start sloughing off if he eats [checks notes] MEAT. ANY KIND OF MEAT. WHAT KIND OF GOD MAKES AN OBLIGATE CARNIVORE THAT'S ALLERGIC TO MEAT?
oh & he also barfs when he purrs too much.
ANYWAY. his breathing is better now but he still clearly has a secondary infection because he has yellow-green nasal discharge that isn't improving with his current antibiotic. he's on methimazole for his thyroid & there's not really a way to tell if that's working without blood work, so we'll do that in 2 weeks. i was supposed to taper him down on prednisolone to only every other day, but now it looks like his skin might be going bad again & that's so hard to control once it starts, so i'm still giving the pred daily (eosinophilic granuloma complex is an autoimmune disease that attacks the skin & pred is an immune suppressant).
i thought i was going crazy cuz to me it looks like the left side of his face - specifically his ear, that bald spot cats have in front of their ear, & his lips - gets kind of red & puffy in the nighttime, but ONLY the left side, & ONLY at night. his left eye also waters. he also has a weird little sore in the crook of his left arm (i mean... left front leg. on the cranial aspect of the left front leg just distal to the elbow, ok? if you wanna get technical).
i took the above photos to show his vet at his next appointment; he's clearly got a fat lippy & he's started developing comedones (cat acne) on his chin. he also just seems dumpy! he's a cat so it's hard to tell but he seems to be sleeping more than usual & is just quiet & not himself. at the appointment with his regular vet i feel like she just kind of brushed off the lymphocytosis, but since that was confirmed by a pathologist & can be a sign of lymphoma or non-viral leukemia, i'm worried about it. the answer is probably that he needs to start seeing an internal medicine specialist again, cuz i'm getting really sick of being passed around the office & subjected to these guessing games. i know that's how veterinary diagnostics work but... i'm just frustrated. they don't follow up or follow through. i was technically supposed to already have a referral to an internist. he was supposed to have an ultrasound like 6 months ago. plus they told me that nobody in town does radioactive iodine treatment for hyperthyroid cats & that's not true.
idk. i'm just writing. i like to talk about veterinary details cuz i guess it helps me feel more in control. i've been working on this cat's cascade of problems for 11 years. god doesn't want this cat to be, but i know better than god. also the vet said "he could have a few more years left" & that really bothered me because he's ONLY 12. i know he's been through a lot but he's gonna live to be 20 at least. all my cats live forever. don't make me think about my cat's mortality when my dog just died last year.
3 notes
·
View notes
Text
Vaccines are the absolute best way to prevent rabies. The reason why rates are so low is because of vaccines. Getting your dog vaccinated against rabies protects them and everyone around them from dying in a particularly horrific manner.
Rabies causes brain tissue to become inflamed, and it causes neurological signals to become mixed up. It’s a terrible disease. All animals with rabies die. And only about 15 humans have survived rabies globally.
Symptoms of rabies are:
🧠 Muscle pain
🧠 Dizziness
🧠 Fatigue
🧠 Fever
🧠 Loss of appetite
🧠 Malaise
🧠 Nausea and vomiting
🧠 Muscle spasms, paralysis and/or weakness
🧠 Numbness or tingling
🧠 Light sensitivity
🧠 Aggression or irritability
🧠 Anxiety
🧠 Difficulty swallowing
🧠 Hypersalivation and drooling
🧠 Headache
🧠 Mental confusion
🧠 Dilated pupils
🧠 Stiff neck
🧠 Seizures
🧠 Coma
🧠 Death
Rabies in dogs and cats can be prevented by a vaccine. Please vaccinate your pets to prevent them from getting this absolutely horrific disease.
"I've decided not to vaccinate my animals. Think about it, how often do you see a rabid dog?"
Yes Heather think about it. Think about how few rabid dogs you see in your comfortable western country with easy access to vet care. Think about why it might be that you've never seen a rabid dog. Really dig deep here you absolute fucking fool.
54K notes
·
View notes
Text
Top 10 Signs Your Pet Needs to Visit the Vet ASAP
As pet parents, we want to give our pets the best care possible, but sometimes it can be hard to know when something is wrong. Our pets can’t speak to tell us when they’re feeling unwell, so it’s essential to look out for certain warning signs. In this guide, we’ll explore the top 10 signs that indicate your pet may need to see a vet right away. Prompt medical attention can make all the difference, and at Vetic, we’re here to ensure your furry family member stays healthy and happy.
Sudden Loss Of Appetite - When your pet suddenly loses interest in food, it could be a sign of an underlying health issue.
What it Means: Loss of appetite in pets can indicate digestive problems, dental issues, or even more severe health concerns like liver disease.
What to Do: If your pet skips more than two meals or is refusing treats, it's time to schedule a check-up.
👉 Book a consultation with our experts at Vetic Pet Clinic Near Me to assess your pet’s health needs.
Excessive Thirst and Urination - While water intake varies, excessive thirst or urination could indicate a problem.
What it Means: Excessive thirst and urination are often symptoms of diabetes, kidney disease, or urinary tract infections.
What to Do: Track your pet’s water consumption, and if it seems unusually high, contact a vet.
Visit us at Vetic Pet Clinic Mumbai for specialized care in diagnosing and treating pet ailments.
Changes in Behavior or Mood - Is your pet acting more aggressive, anxious, or lethargic? Behavioral shifts often signal health issues.
What it Means: Mood changes can indicate pain, stress, or even neurological issues. For example, an otherwise friendly dog may growl if experiencing discomfort.
What to Do: Take note of any drastic changes and seek veterinary help if the new behavior persists.
You can find professional pet consultations at Vetic—check out our services here.
Persistent Vomiting or Diarrhea - Occasional vomiting is common, but frequent episodes warrant attention.
What it Means: Persistent vomiting or diarrhea can indicate gastrointestinal issues, infections, or even toxic ingestion.
What to Do: If your pet has been vomiting or experiencing diarrhea for more than 24 hours, visit the vet immediately.
Coughing, Sneezing, or Breathing Difficulties - Respiratory symptoms should never be ignored, especially if they’re new or severe.
What it Means: Coughing, sneezing, or difficulty breathing could be symptoms of allergies, respiratory infections, or even heart disease.
What to Do: If your pet is struggling to breathe or showing signs of respiratory distress, seek urgent care.
Schedule an appointment at Vetic Pet Clinic Near Me to get a proper diagnosis and treatment plan.
Skin Issues: Redness, Rashes, or Hair Loss - Skin problems can be a sign of allergies or infections and are often accompanied by scratching or discomfort.
What it Means: Redness, rashes, or hair loss can signal allergies, skin infections, or parasites like fleas and mites.
What to Do: If the skin issue persists or worsens, consult a vet for treatment options.
Limping or Difficulty Moving - If your pet suddenly starts limping or has trouble moving, it’s time for a vet check-up.
What it Means: Limping or reduced mobility can stem from injury, arthritis, or other orthopedic conditions.
What to Do: Limit physical activity and schedule an immediate visit to the vet to prevent further damage.
Unusual Lumps or Bumps - Finding lumps or bumps on your pet’s body can be alarming, but not all are harmful.
What it Means: Some lumps are benign, but others could indicate infections or tumors.
What to Do: It’s best to have any lump checked by a vet to determine whether further action is necessary.
Bad Breath or Excessive Drooling - Oral health problems often go unnoticed, but bad breath and drooling are key indicators.
What it Means: Dental issues, infections, or digestive issues could be behind these symptoms.
What to Do: Regular dental check-ups and oral hygiene can prevent these issues, but a vet visit is recommended if symptoms are ongoing.
Sudden Weight Loss or Gain - Unexplained changes in weight are often linked to health issues.
What it Means: Rapid weight loss or gain can indicate diabetes, thyroid issues, or other metabolic disorders.
What to Do: Monitor your pet’s weight regularly and consult a vet if you notice significant changes.
When in Doubt, Visit Vetic
Your pet’s health is always our priority at Vetic. If you’ve noticed any of the signs above, don’t wait! Early intervention is the best way to keep your pet happy and healthy. Schedule a consultation today to ensure your pet’s well-being.
👉 Book an appointment at Vetic Pet Clinic Near Me or explore our full list of services in Mumbai at Vetic Pet Clinic Mumbai.
Prioritize your pet’s health today! Visit Vetic for comprehensive care from compassionate veterinarians.
0 notes
Text
Top 5 Neurological Diseases in Dogs
Learn about common neurological diseases in dogs, their symptoms, and treatment. Discover ways to improve your dog's quality of life today.
Welcoming a puppy as the newest addition to your family can be a truly exciting and unforgettable feeling. You’d have tremendous love for that pup, as you’ll be its whole life, while it is going to be a part of the best decade of yours. As pet owners, we hate to think about our pets getting sick or dying, however, that’s only natural. What’s not natural, and is often heartbreaking is to see our…
#Dog Diseases#Dog Protection Advice#doggozila#healthy doggos lifestyle#Healthy Dogs Topics#improve your dog health#Top Dog Health Tips#Vet Tips
0 notes
Text
Top 5 Neurological Diseases in Dogs
Learn about common neurological diseases in dogs, their symptoms, and treatment. Discover ways to improve your dog's quality of life today.
Welcoming a puppy as the newest addition to your family can be a truly exciting and unforgettable feeling. You’d have tremendous love for that pup, as you’ll be its whole life, while it is going to be a part of the best decade of yours. As pet owners, we hate to think about our pets getting sick or dying, however, that’s only natural. What’s not natural, and is often heartbreaking is to see our…
#Dog Diseases#Dog Protection Advice#doggozila#healthy doggos lifestyle#Healthy Dogs Topics#improve your dog health#Top Dog Health Tips#Vet Tips
0 notes
Text
stop sharing these "dancing dog" videos. this dog is grimacing and stumbling and dirty, this is an example of a street dog with advanced canine distemper whose neurological system is falling apart. it's extremely common in China and India, but present everywhere, and there are regular outbreaks in the USA. you need a routine vaccination to prevent it. this dog has not been vaccinated, and is dying. sorry to ruin the funny animal video, the people in this video also just think the dog is funny and aren't aware that it's in pain or end stage terminal disease.
here's another example from Gambia. the name of the symptom that causes the dancing/bouncing is "myoclonus".
#tw animal suffering#canine distemper#tw animal death#debunk#i know people dont know better but im sick of seeing it#its vaguely possible this is a distemper survivor but based on the context i dont think thats the case#its myoclonus either way and not voluntary movement
4K notes
·
View notes
Text
Veterinary Vaccine: Importance of Vaccines for Our Furry Friends
Veterinary Vaccines are Essential for Pets Vaccines play a crucial role in keeping our pets healthy. Just like humans, pets are susceptible to various infectious diseases that can make them severely ill and sometimes even lead to death. Vaccines help boost pets' immune system and provide protection against dangerous diseases. The most common and important vaccines recommended for dogs and cats include: Rabies Vaccine Rabies is a fatal viral disease that can infect both pets and humans. It is transmitted through the bite of an infected animal. According to experts, rabies vaccination is absolutely necessary to protect our furry friends from this threat. In many countries and regions, it is mandatory by law to vaccinate pets against rabies to prevent its spread in the community. Pets require an initial series of rabies vaccines starting at 3 months of age followed by regular booster shots as per the schedule recommended by veterinarians. This ensures lifelong protection against this fatal yet preventable disease. Core Vaccines for Dogs Dogs need a series of core vaccines early in their life and regular boosters to maintain protection. The core Veterinary Vaccines routinely recommended for dogs include: - Distemper: This viral disease can cause seizures, neurological issues and fatality in dogs if not vaccinated. Puppies require a series of distemper vaccines starting from 6-8 weeks of age with boosters every year. - Parvovirus: This highly contagious virus often leads to severe vomiting, diarrhea and even death in unvaccinated puppies. An initial series along with annual boosters are necessary to shield dogs from parvo. - Adenovirus: Also known as hepatitis, this infection can cause liver failure in dogs. Core vaccines effective in preventing adenovirus contain both types 1 and 2. - Parainfluenza: This respiratory virus can lead to pneumonia if not vaccinated against. It is included in combination vaccines for dogs. Core Vaccines for Cats Like dogs, cats also require a set of core vaccines for comprehensive protection. The most essential ones for felines include: - Panleukopenia: Also known as feline distemper, it can result in lethal gastrointestinal issues in cats if not vaccinated. Kittens need an initial series starting at 6-8 weeks with a booster at 1 year. - Calicivirus: Veterinary Vaccines highly contagious virus leads to flu-like symptoms and pneumonia in cats. Vaccination is done along with panleukopenia vaccine. - Rhinotracheitis virus: As the name suggests, it can cause upper respiratory infection in cats. Core feline vaccines contain this virus along with panleukopenia and calicivirus. Optional Vaccines In addition to the core ones, veterinarians may also recommend some non-core or optional vaccines depending upon the pet's lifestyle, risk of exposure and local disease situation. These include: For Dogs: - Leptospirosis: Spread through contact with infected urine, it can damage organs. Recommended only in high-risk areas. - Lyme disease: Transmitted through tick bites, it causes joint issues. Dogs in wooded/grassy areas may need this vaccine. For Cats: - Chlamydophila: Bacterial infection leading to conjunctivitis. Indoor cats at low risk do not always require this vaccine. - Rabies: Core for dogs but optional for indoor cats in low-rabies regions after discussing risks with vet.
Get more insights on Veterinary Vaccines
About Author:
Money Singh is a seasoned content writer with over four years of experience in the market research sector. Her expertise spans various industries, including food and beverages, biotechnology, chemical and materials, defense and aerospace, consumer goods, etc. (https://www.linkedin.com/in/money-singh-590844163)

#Veterinary Vaccines#Animal Health#Pet Vaccines#Livestock Immunization#Animal Disease Prevention#Veterinary Medicine#Animal Care#Veterinary Immunology
0 notes